Development of a human organoid biofilm model that can mimic skin and soft-tissue infections
Human skin is a very complex organ and is home to a diverse community of commensal microbes. The ability to study skin infections in the lab could give valuable insights into the development of new therapies.
The compromise in infection research
To truly understand how bacteria cause skin and soft tissue infections (SSTIs) in patients, we need to accurately mimic what happens during an infection in the lab. If we can’t do this, then we run the risk of drawing false conclusions that could set back efforts to develop new therapies. While we can’t just grow bacteria shaking in a flask and pretend that this is an accurate depiction of the infection process, we must also be pragmatic. Discoveries need to come from the lab; this is where researchers can do experiments, test hypotheses and crucially, fail safely. Finding a middle ground that can give us real insights into the infection process and can be easily set up in the lab is the holy grail of infection biology research.
Recently, a team of researchers proposed a human organoid model for assessing antibiofilm activity. The understated genius of this approach is that it attacks infection from three different angles that are frequently present in infections and missing from laboratory studies(1)
Investigating biofilms
Firstly, they look at biofilms that cause 65% of all SSTIs. This bacterial “lifestyle” affects how the microbial cells interact with the human immune system as well as antibiotics. This makes the bacteria in biofilms harder to kill.
If we ignore biofilms and use standard cultures, there is a high probability that we will draw the wrong conclusions from research.
Investigating how to disrupt biofilms
The most common approach to look for novel antimicrobial compounds is to find something that will kill the bacteria, or at least prevent them from growing. As it happens, this approach could be more limited than it needs to be. If biofilms make bacteria harder to kill, then compounds that can break them up, or prevent biofilms from forming will make it easier for the human immune system to clear the infections.
It will also make it more likely that currently available antibiotics will work once the biofilm is no longer present. Thinking laterally about the treatment of infections to include biofilm treatment gives us more choice of compounds and reduces the risk of developing antimicrobial resistance.
Growing them in a human organoid
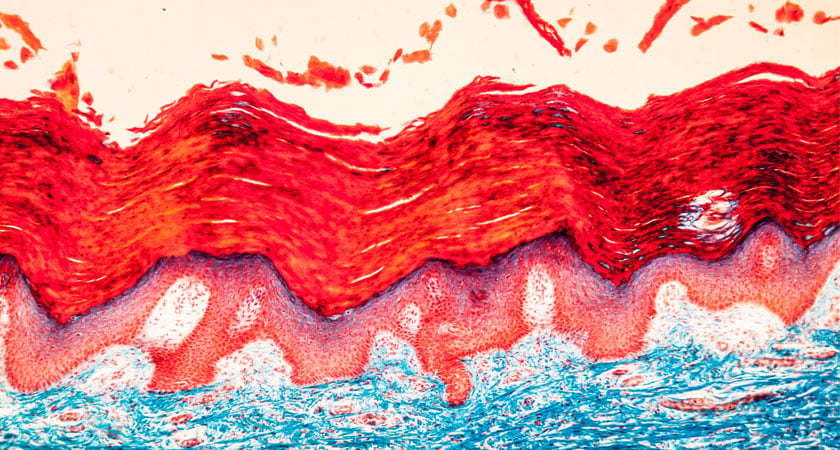
The research paper describes a human epidermis organoid model to simulate the conditions that bacteria would find on the skin. By doing this, they were able to simulate a skin burn, which is a serious risk factor for staphylococcal infections.
The findings
Using this model, the team showed that a synthetic antibiofilm peptide was able to significantly reduce the bacterial burden in the model. Crucially, a novel peptide reduced the bacterial load to a greater extent that murpirocin, which is the topical antibiotic of choice for staphylococcal infections.
Crucially for the accuracy of the model, ThinCert® allows you to create an air-liquid interface inside a single well.
This skin model can then be used to host a biofilm layer on top to closely simulate a real infection. As this can be done many times in the same multi-well plate then it is also possible to perform large numbers of replicates to uncover new therapies with a lot of statistics to back them up.
Not only can this model help to identify model therapeutic compounds, it can also do it without the need for animal models. The importance of testing drugs in animals is currently being rigorously examined, but how similar are humans and rodents really?
If we can find ways to find new antimicrobials more ethically and accurately, then these options should be fully explored.
Ready to enter the next level?
Please fill out this form and contact our experts today to find the perfect solution for you!
Don't miss our regular updates on scientific topics around 3D Cell Culture
References
[1] Wu, B., Haney, E.F., Akhoundsadegh, N. et al. Human organoid biofilm model for assessing antibiofilm activity of novel agents. npj Biofilms Microbiomes 7, 8 (2021)