Importance of Realistic Tumoroid Models in Cancer Drug Screening
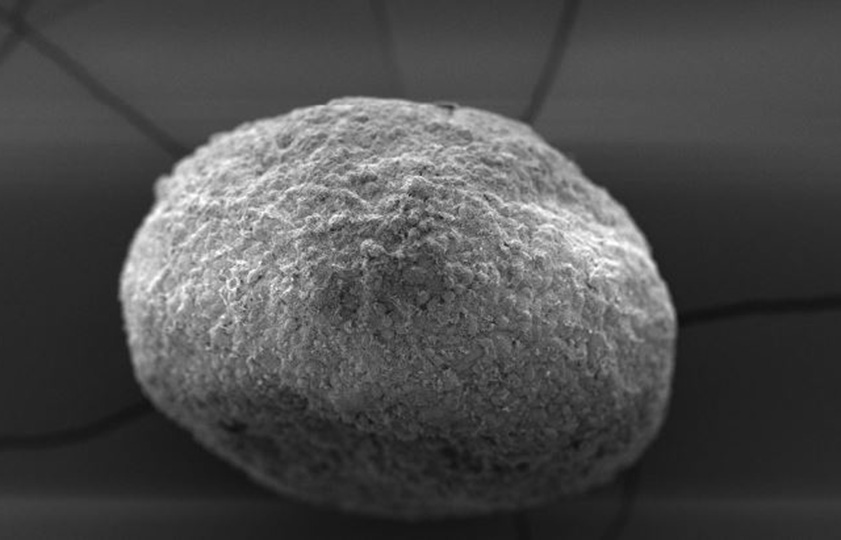
Tumoroids (“tumor-like organoids”) are valuable tools in personalized medicine.
They are being refined to include vascularization to study the role of angiogenesis in cancer development and drug targeting and address the problems of failure in anti-cancer drug screens and resistance to treatment.Tumoroids: valuable tools in cancer research and translational medicine
The fight against cancer is aided by model systems supporting basic research into tumor biology and the tumor microenvironment (TME), cancer drug development, translational research, and personalized medicine, including functional drug screening. Achieving this has involved a shift from 2D to 3D cell cultures to increase the dimensionality of cell-cell interactions, providing a phenotype that can recapitulate in vivo biology but can be performed in vitro (1).
Tumoroids are now regarded as being comparable to laborious patient-derived xenograft (PDX) models and the in vivo environment (2). Tumoroids are essentially “tumor-like organoids” that are typically prepared using cells from primary tumors harvested from patients and can therefore mimic the microenvironment of a specific tumor. They are a better predictive drug discovery tool than 2D models, and they show promise in guiding personalized medicine, including immunotherapy (3, 4, 5).
A key role in personalized medicine and drug screening
Tumoroids prepared from the tumors of individual patients are valuable tools in cancer research. They also have great potential in personalized medicine, for example, drug screens to identify effective drugs against individual tumors. Patient-derived tumoroids (PDT) have two major advantages:
1. They retain key characteristics of the original tumor, including morphology, genomic profiles, and mutations, thus recapitulating the genetic and phenotypic heterogeneity.
2. The PDT approach enables the rapid generation of an informative model system, which is critical when screening drugs for individual patients (days or weeks compared to months for PDX).
One example of the value of tumoroids in personalized medicine is a study on lung cancer (6), a cancer form that shows substantial genetic and phenotypic heterogeneity across individuals, making it a particularly interesting target for personalized medicine. Tumoroids and normal bronchial organoids were readily established from patient tissues and recapitulated the original tissue architecture and genomic alterations. The tumoroids could then be used to predict patient-specific drug responses.
Refining the tumor model
Mimicking the natural TME requires more than 3D models based on cancer cell lines. The TME comprises extracellular matrix (ECM), stromal cells, and lymphatic vascular networks. Different tumor types may require special approaches, as exemplified below.
Establishing an air-liquid interface
When establishing lung tissue and tumor models, generally it requires the air-liquid interface (ALI) to promote the differentiation of airway epithelial cells. Tumoroids cultured at the ALI can, for example, be used in the study of aerosol-based drug delivery (7). Lung organoids generated on permeable membranes that provide an ALI are also valuable in research on respiratory toxicants and pathogens, including SARS-CoV-2 causing COVID-19 (8, 9).
Incorporating vascularization to research and target angiogenesis
Poor drug transport and delivery, which can depend on both the microvessel network of the TME and the vascularization around the tumor, are major causes of failure in anti-cancer drug screens and resistance to treatment. Not only that, the process of angiogenesis during tumor progression is itself a target for drug development (10), and the effects of drugs or genetic manipulations on sprouting angiogenesis can be measured using the spheroid-based sprouting assay (11,12, 13). Including vascularization within and around the PDT is therefore essential to accurately recapitulate in vivo conditions.
In the second article in this series, we will look at an example of how vascularization can be incorporated into a PDT model to ensure that the TME and its surroundings are replicated as quickly and accurately as possible for functional drug screening.
Don't miss out on important updates! Stay informed about new trends and insights in 3D cell culture and subscribe to our blog series now!
Ready to enter the next level?
Please fill out this form and contact our experts today to find the perfect solution for you!
Don't miss our regular updates on scientific topics around 3D Cell Culture
References
[1] Souza GR, Spicer T. SLAS special issue editorial 2022: 3D cell culture approaches of microphysiologically relevant models. SLAS Discov. 2022 Apr;27(3):149-150. doi: 10.1016/j.slasd.2022.03.006. Epub 2022 Mar 24. PMID: 35339725.[2]Pape J, Emberton M, Cheema U. 3D Cancer Models: The Need for a Complex Stroma, Compartmentalization and Stiffness. Front Bioeng Biotechnol. 2021 Apr 12;9:660502. doi: 10.3389/fbioe.2021.660502. PMID: 33912551; PMCID: PMC8072339.
[3]Xu H, Lyu X, Yi M, Zhao W, Song Y, Wu K. Organoid technology and applications in cancer research. J Hematol Oncol. 2018 Sep 15;11(1):116. doi: 10.1186/s13045-018-0662-9. PMID: 30219074; PMCID: PMC6139148.
[4]Gunti, S.; Hoke, A.T.K.; Vu, K.P.; London, N.R., Jr. Organoid and Spheroid Tumor Models: Techniques and Applications. Cancers 2021, 13, 874. https://doi.org/10.3390/cancers13040874
[5]Tatullo M, Marrelli B, Benincasa C, Aiello E, Makeeva I, Zavan B, Ballini A, De Vito D, Spagnuolo G. Organoids in Translational Oncology. J Clin Med. 2020 Aug 27;9(9):2774. doi: 10.3390/jcm9092774. PMID: 32867142; PMCID: PMC7564148.
[6]Kim M, Mun H, Sung CO, Cho EJ, Jeon HJ, Chun SM, Jung DJ, Shin TH, Jeong GS, Kim DK, Choi EK, Jeong SY, Taylor AM, Jain S, Meyerson M, Jang SJ. Patient-derived lung cancer organoids as in vitro cancer models for therapeutic screening. Nat Commun. 2019 Sep 5;10(1):3991. doi: 10.1038/s41467-019-11867-6. PMID: 31488816; PMCID: PMC6728380.
[7]Man F, Tang J, Swedrowska M, Forbes B, T M de Rosales R. Imaging drug delivery to the lungs: Methods and applications in oncology. Adv Drug Deliv Rev. 2023 Jan;192:114641. doi: 10.1016/j.addr.2022.114641. Epub 2022 Dec 9. PMID: 36509173.
[8]Cao X, Coyle JP, Xiong R, Wang Y, Heflich RH, Ren B, Gwinn WM, Hayden P, Rojanasakul L. Invited review: human air-liquid-interface organotypic airway tissue models derived from primary tracheobronchial epithelial cells-overview and perspectives. In Vitro Cell Dev Biol Anim. 2021 Feb;57(2):104-132. doi: 10.1007/s11626-020-00517-7. Epub 2020 Nov 11. PMID: 33175307; PMCID: PMC7657088.
[9]Djidrovski I, Georgiou M, Hughes GL, Patterson EI, Casas-Sanchez A, Pennington SH, Biagini GA, Moya-Molina M, van den Bor J, Smit MJ, Chung G, Lako M, Armstrong L. SARS-CoV-2 infects an upper airway model derived from induced pluripotent stem cells. Stem Cells. 2021 Oct;39(10):1310-1321. doi: 10.1002/stem.3422. Epub 2021 Jun 21. PMID: 34152044; PMCID: PMC8441770.
[10]Qi S, Deng S, Lian Z, Yu K. Novel Drugs with High Efficacy against Tumor Angiogenesis. Int J Mol Sci. 2022 Jun 22;23(13):6934. doi: 10.3390/ijms23136934. PMID: 35805939; PMCID: PMC9267017.
[11]Heiss M, Hellström M, Kalén M, May T, Weber H, Hecker M, Augustin HG, Korff T. Endothelial cell spheroids as a versatile tool to study angiogenesis in vitro. FASEB J. 2015 Jul;29(7):3076-84. doi: 10.1096/fj.14-267633. Epub 2015 Apr 9. PMID: 25857554.
[12] Kannan P, Schain M, Lane DP. An Automated Quantification Tool for Angiogenic Sprouting From Endothelial Spheroids. Front Pharmacol. 2022 Apr 27;13:883083. doi: 10.3389/fphar.2022.883083. PMID: 35571133; PMCID: PMC9093605.
[13]Daquinag AC, Souza GR, Kolonin MG. Adipose Tissue Engineering in Three-Dimensional Levitation Tissue Culture System Based on Magnetic Nanoparticles. Tissue Eng Part C, 19: 336-44, 2013.